This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
N.sahithi
Roll no -107
Case history-
A 45 years old male came with
-c/o Abdominal distension since 4months
- SOB On and off since 4 months
History of presenting illness-
Patient was apparently asymptomatic 4 months back then he developed abdominal distension which was ,Insidious in onset, gradually progressive in nature .
Since 1 month abdominal distension is progressive in nature for which he visited government hospital was diagnosed as ALD with portal Hypertension with Decompensated liver disease with Hepatic encephalopathy Grade 1 with Right pleural effusion mild.
Pedal edema since 4 months insidious in onset gradually progressive ,relieved at night and aggrevated in morning (pitting type).
Sob present even at rest,orthopnea,PND present.
No chest pain , palpitations.
C/o decreased urine output since 1 month since then patient is on Foleys catheter and 2 lit ascitic tap was done
PAST HISTORY
K/c/o Type 2 DM since 15 years and on medications
Operated for iliospoas Abscess 10 months ago
Not a K/C/0 HTN,CAD, EPILEPSY, ASTHMA, TB , CVA ,THYROID DISORDERS
PERSONAL HISTORY -
Appetite: Normal
Diet-mixed
Bowel-Regular
Bladder- Decreased urine output since 1 month
Addictions:
Regular alcoholic since 15yrs
Occassional alcoholic since 4yrs (1- 2 times/ month)
2months ago patient consumed alcohol for 10days continuously
General examination-
No pallor ,icterus, cyanosis, clubbing , lymphadenopathy
Vitals-
Bp -110/70 mm hg
PR-96bpm
Temp-96.4 f
RR- 18cpm
SPO2- 98%on RA
Grbs - 125mg/dl
Systemic examination-
CVS-s1, s2 heard , no murmurs
RS-BAE present
CNS- No focal neurological deficit
P/A- Inspection:
Round, with distention
Umbilicus: protruded
No visible pulsation,peristalsis, dilated veins and localized swellings.
Palpation:
Soft, distended, non tender
No signs of organomegally
Percussion:
fluid thrill present
Auscultation:
Bowel sounds heard .
Diagnosis:
Chronic Decompensated liver disease with k/c/o Dm ll since 15yrs.
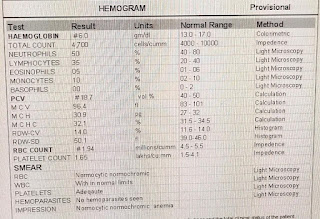
Investigations:
 |
|
|
|
|
Fever chart:
Therapeutic

Treatment:
1.INJ Optineuron 1amp+100ml Ns /iv/OD
2.Tab lasilactone 20/50mg po BD 8am --- 4pm
3.syp.lactulose 15ml po BD
4.syp Hepamerz 10ml po BD
5.High protein diet 2 egg whites/ day
6.protein powder 2tsps in 1 glass of water TID
7.Fluid restriction <2lit /day
8.salt restriction <2g /day
Follow up:
On 30/04/23
S
C/o abdominal distention (discomfort), shortness of breath present (reduced)
Stools not passed
O:
Patient is conscious coherent and cooperative
pallor - present ,pedal edema present
No icterus , clubbing, cyanosis,lymphadenopathy
Vitals :
BP- 140/80mmhg
PR -82bpm
RR-28cpm
Spo2 99% at room air
GRBS - 110mg/dl
Temperature 98°F
I/O :- 950ml/1150 ml
Cvs: s1,s2 heard ,no Murmurs,jvp not raised
Rs: BAE,no added sounds ,NVBS,
P/A: soft, distended, bowel sounds can be heard, fluid thrill present
CNS:
Pt is conscious,
Speech is normal
No meningeal signs
Normal cranial nerve examination, motor system, sensory system
Gcs: E4,V5,M6
Reflexes:
R L
B ++ ++
T ++ ++
S ++ ++
K ++ ++
A ++ ++
P Flexor Flexor
A:
Chronic decompensated liver disease ( since 4 months)
K/c/o DM type 2 since 15 yrs
Anemia under evaluation
Chronic kidney disease
P:
1.fluid restriction < 2L/day
2.salt restriction < 2g/day
3.INJ. optineuron 1amp +100 ml NS/IV/OD
4.Tab spiranolactone 25mg/po/bd
5.syp lactulose 10ml/po/tid
6.high protein diet 2egg whites/day
7.protein powder 2tsps in 1 glass of water /po/tid
8.strict I/O charting
9.vitals monitoring 4th hourly
10.GRBS monitoring 6th hourly
On 01/05/24
-
S
C/o abdominal distention (discomfort), shortness of breath present (reduced)
Stools not passed
O:
Patient is conscious coherent and cooperative
pallor - present ,pedal edema present
No icterus , clubbing, cyanosis,lymphadenopathy
Vitals :
BP- 140/80mmhg
PR -84bpm
RR-18cpm
Spo2 98% at room air
GRBS - 182mg/dl
Temperature 98°F
I/O :- 900ml/1550 ml
Cvs: s1,s2 heard ,no Murmurs,jvp not raised
Rs: BAE,no added sounds ,NVBS,
P/A:
Inspection:
Round, with distention
Umbilicus: Inverted
No visible pulsation,peristalsis, dilated veins and localized swellings.
Palpation:
Soft, distended,non tender
No signs of organomegally
Percussion:
fluid thrill, shifting dullness present
Ascultation: bowel sounds can be heard
CNS:
Pt is conscious,
Speech is normal
No meningeal signs
Normal cranial nerve examination, motor system, sensory system
Gcs: E4,V5,M6
Reflexes:
R L
B ++ ++
T ++ ++
S ++ ++
K ++ ++
A ++ ++
P Flexor Flexor
A:
Acute on Chronic decompensated liver disease
Normocytic Normochrimic Anaemia (Hypoproliferative)
?Anemia of chronic disease
HRS-Chronic kidney disease ? Diabetic Nephropathy with ? Porto pulmonary HTN
P:
1.fluid restriction < 2L/day
2.salt restriction < 2g/day
3.INJ. optineuron 1amp +100 ml NS/IV/OD
4.Tab spiranolactone 2t5mg/po/bd
5.Tab udiliv 300mg/PO/BD
6.T.Rifagut 550mg/PO/BD
7.syp lactulose 10ml/po/tid
8. Syp.Hepamerz 10ml/PO/BD
8.high protein diet 2egg whites/day
9.protein powder 2tsps in 1 glass of water /po/tid
10.Inj.vit k 1amp +100ml IV/OD
11.strict I/O charting
12.vitals monitoring 4th hourly
13.GRBS monitoring 6th hourly
02.05.2023
S
C/o abdominal distention (discomfort), shortness of breath present (reduced)
2episodes of stools passed
O:
Patient is conscious coherent and cooperative
pallor - present ,pedal edema present
No icterus , clubbing, cyanosis,lymphadenopathy
Vitals :
BP- 140/100mmhg
PR -90bpm
RR-20cpm
Spo2 98% at room air
GRBS - 131mg/dl
Temperature 98°F
I/O :- 750ml/500 ml
Cvs: s1,s2 heard ,no Murmurs,jvp not raised
Rs: BAE,no added sounds ,NVBS,
P/A: soft, distended, mild tenderness in both iliac fossa
CNS:
Pt is conscious,
Speech is normal
No meningeal signs
Normal cranial nerve examination, motor system, sensory system
Gcs: E4,V5,M6
Reflexes:
R L
B ++ ++
T ++ ++
S ++ ++
K ++ ++
A ++ ++
P Flexor Flexor
A:
Acute on Chronic decompensated liver disease
Normocytic Normochrimic Anaemia (Hypoproliferative)
?Anemia of chronic disease
HRS-Chronic kidney disease ? Diabetic Nephropathy with ? Porto pulmonary HTN
P:
1.fluid restriction < 2L/day
2.salt restriction < 2g/day
3.INJ. optineuron 1amp +100 ml NS/IV/OD
4.Tab spiranolactone 25mg/po/bd
5.syp lactulose 10ml/po/tid
6.high protein diet 2egg whites/day
7.protein powder 2tsps in 1 glass of water /po/tid
8.Inj.vit k 1amp +100ml IV/OD
9.strict I/O charting
10.vitals monitoring
11.GRBS monitoring 6th hourly
12.Tab Clinidipine 10mg po/od















Comments
Post a Comment